SYSTEM ARCHITECTURE
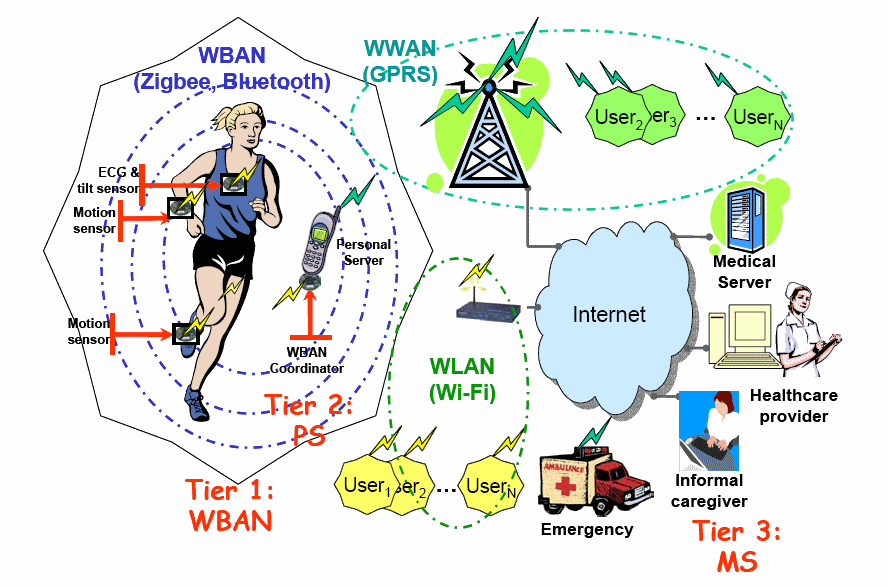
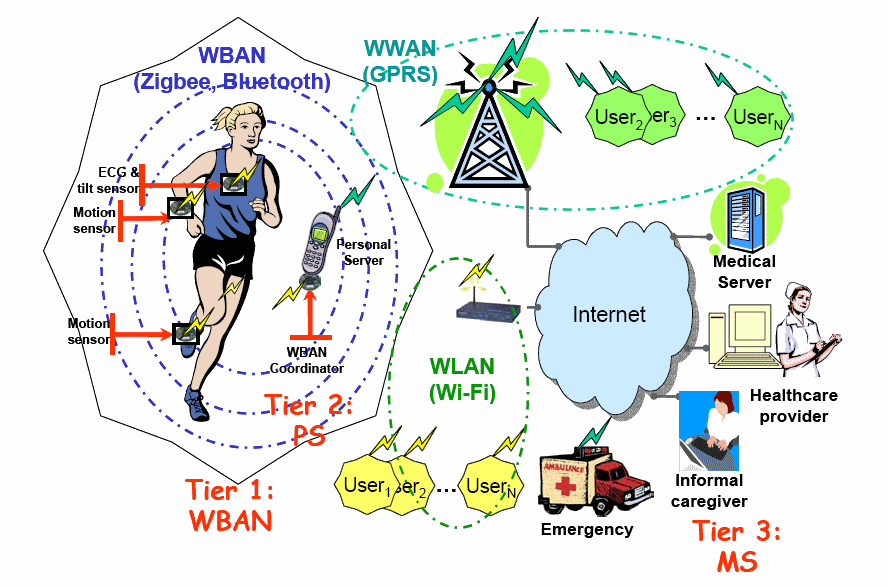
Figure 6 shows a multi-tier health monitoring system based on WBAN . Typically, a WBAN will form the lowest tier (Tier 1) of a multi-tier medical information system for health monitoring. The system is composed of three tiers.
a) Biosensors - For monitoring of vital physiological signs (oxygen level in the blood,
heart rate, body temperature ,rate of respiration etc). For example, an electro- cardiograph (EKG) sensor can be used for monitoring heart activity of cardiac patients during a rehabilitation period at home. The heart sensor can operate in multiple modes reporting either (i) a raw ECG signal (from one or multiple channels), (ii) time-stamped heart beats, or (iii) averaged heart rate over a certain period of time.
b) Motion sensors - For collection of information about the current state of the patient's body (walking, running, standing, sitting, falling etc). The motion sensors, each equipped by a 3-D accelerometer, can also operate in several modes reporting either (i) raw acceleration signals for X, Y, and Z axes, (ii) extracted features (e.g., time-stamped steps or phases of a step), or (iii) an estimated level of activity (e.g., AEE -activity induced energy expenditure over a certain period of time). The WBAN sensor nodes together with a WBAN network coordinator collect data and pass it through the wireless Personal Device (PD) or smart phone.
In this design, a sophisticated sensor is integrated into the WBAN called Medical Super Sensor (MSS). This sensor has more memory, processing and communication capabilities than other sensor nodes. MSS uses a radio frequency to communicate with other body sensors. ZigBee is used as a communication protocol to communicate with the Personal Server. Medical Super-Sensor (MSS) unobtrusively samples, collects multiple sensed vital signs by the body sensors, filtering out all redundant data thereby reducing large volume of data transmitted by BSNs, store them temporarily, process and transfer the relevant patient's data to a personal server through wireless personal implemented using ZigBee/IEEE 802.15.4. This improves overall bandwidth utilization as well as reducing power consumption of the BSs because each nodes does not need to transmit sensed data to the IPDA but to the collector which is MSS and it is closer to the BSs than IPDA and extending battery life of each sensor node
Tier 2 encompasses the Personal Server (PS) application. The personal server interfaces the WBAN nodes through a communication protocol using ZigBee. It is implemented on an IPDA. The PS provides a transparent interface to the wireless sensor nodes, an interface to the user, and an interface to the medical server. It holds patient authentication information and is configured with the medical server IP address in order to interface the medical services. Once the WBAN network is configured, the PS application manages the network and takes care of channel sharing, time synchronization, data retrieval and processing, and fusion of the data.
Based on synergy of information from multiple physiological, location, activity, and environmental sensors; the PS application can determine the user's state and his or her health status; The IPDA has the capability to perform the task of analyzing the physiological data intelligently and do a local reasoning to determine user's health status based on data received from MSS and provide feedback through a user friendly and interactive graphical user interface. Finally, if a communication channel to the medical server is available, the PS can establish a secure link to the medical server and send condensed or detailed reports about the user's health status. These reports can be processed, displayed, and integrated into the user's medical record. However, if a link between the PS and the medical server is not available, the PS should be able to store the data locally and initiate data uploads when a link becomes available. Depending on the use scenario, the PS application can run on a smart phone (as illustrated in Figure 1), or a Wireless Wide Area Network (WWAN)-enabled Personal Digital Assistant (PDA), or on a home personal computer.
Tier 3 includes a medical server accessed via the Internet and is called the Medical Server for Healthcare Monitoring (MSHM). It is the responsibility of the medical server to authenticate users, accept health monitoring session uploads, format and insert the session data into corresponding medical records, analyze the data patterns, recognize serious health anomalies in order to contact emergency care givers, and forward new instructions to the users, such as physician prescribed exercises.
The medical server keeps electronic medical records of registered users and provides various services to the users, medical personnel, and informal caregivers. The patient's physician can access the data from his/her office via the Internet and examine it to ensure the patient is within expected health metrics (heart rate, blood pressure, activity), ensure that the patient is responding to a given treatment or that a patient has been performing prescribed exercises. A server agent may inspect create an alert if the received data is out of range (i.e. deviation from threshold) or recognize serious health anomalies condition, medical staff in the emergency unit can be notified to take necessary actions.
WBAN environments pose information challenges that are typical in clinical monitoring environments. Performance characteristics of typical wireless sensors, such as processing power and available memory, severely limit real-time capabilities of a typical WBAN. In addition, a personal server must have (a) enough local storage to log hours of sensor data and (b) the ability to upload these data wirelessly to a remote medical record repository using the Internet when a hub becomes available. At this point, the data will be available for remote access by physicians and researchers that wish to extract physiological parameters, apply state-of-health assessment algorithms, note trends in patient data over time, and even predict health crises. Additionally, WBANs will be assembled and configured by the patients themselves, which imposes ease-of-use constraints on the user interface and implies access to a different class of help resources. This point of care systems must also utilize the same information exchange standards and nomenclature rules employed by the hospital information network if these data are to integrate seamlessly into a patient's electronic medical record. Finally, these wearable systems must be reconfigurable at the device level to accommodate different monitoring needs. This means that the personal server must be able to update its local device registry 'on-the-fly' and alter the lengths of its transmission packets depending on the number and type of sensors worn by the patient. Typical reconfiguration scenarios include (1) system assembly and disassembly (e.g., for a bath or exercise in a pool), (2) sensor removal (e.g., to change batteries or switch out a poorly functioning device), (3) sensor addition (e.g., adding a pulse oximeter to identify desaturation events during exercise or sleep), and (4) changing a sensor's operational mode (e.g., asking it to send raw data rather than calculated parameters). Some types of sensor nodes may acquire large quantities of medical information in real-time. Subsequently, data must be sent to the host for storage or post-processing from time to time. Since wireless transmission is relatively energy costly, the gateway should only transmit context relevant data when needed, to minimize energy consumption.
In addition to the above the requirements and challenges for a well-designed BAN include wide variability of data rates, the restricted energy consumption, the need for quality of service and reliability, ease-of-use by medical professionals and security and privacy issues as discussed below:
a) Form factor - Size and weight are very important for BAN sensors, as they directly affect the comfort of the patient. The smaller the area and mass of a node, the fewer restrictions it will introduce on the patient's activities. However, this must be balanced against the requirements for sensor signal-to-noise ratio, noise immunity and efficiency of the antenna for the wireless communications link. As companies look at targeting BANs toward consumer applications, user-friendliness and reliability are both important factors for increased adoption.
b) Power and current consumption. Battery life is a critical challenge in BAN node design. The need for frequent replacement or recharging of batteries is undesirable for wearable nodes and unacceptable for many implantable nodes Several techniques, such as sensor and communication duty cycling and the use of super-regenerative radio receivers are making strides toward longer operational times and battery autonomy . Some designers are looking toward new developments in energy harvesting techniques to extend the lifetime of their BAN products. A TDMA-based MAC protocol is energy efficient and flexible in terms of bandwidth allocation and supporting a sleep mode by exploiting specific characteristics of WBANs.
c) Quality of service and Reliability. When dealing with medical devices and applications, it is imperative to have a system that provides sufficient data accuracy and unquestioned data reliability. Proper quality of service (QoS) handling is an important part in the framework of risk management of medical applications. A crucial issue is the reliability of the transmission in order to guarantee that the monitored data is received correctly by the health care professionals. The reliability can be considered either end-to-end or on a per link base. Examples of reliability include the guaranteed delivery of data (i.e. packet delivery ratio), in-order-delivery; moreover, messages should be delivered in reasonable time. The reliability of the network directly affects the quality of patient monitoring and in a worst case scenario it can be fatal when a life threatening event has gone undetected. Patient safety depends on the repeatability, accuracy and reliability of a BAN system at the sensing and wireless transmission levels.
d) Security. The communication of health related information between sensors in a WBAN is subject to the following security requirements: data confidentiality, data authenticity, data integrity and data freshness. Data confidentiality means that the transmitted information is strictly private and can only be accessed by authorized persons, e.g. the doctor attending the patient. It is usually achieved by encrypting the information before sending it using a secret key and can be both symmetrically and asymmetrically. Data authenticity provides a means for making sure that the information is sent by the claimed sender. For this, a Message Authentication Code (MAC) is calculated using a shared secret key. Data integrity makes sure that the received information has not been tampered with. This can be inspected by verifying the MAC. Data freshness guarantees that the received data is recent and not a replayed old message to cause disruption. A much used technique is to add a counter which is increased every time a message is sent.
Because WBAN systems and their supporting infra-structure are geographically distributed, they present a greater challenge in the areas of throughput, data integrity, and data security when compared to traditional clinical systems. There are issues of patient protection that become important. To protect patient privacy and prevent hacking into the network, BAN nodes must implement adequate security measures.
Patient and data protection require the integration of services to (a) verify the identity of the WBAN wearer (i.e., authentication), (b) protect the confidentiality of the wearer, (c) establish and maintain secure links between the wearer and their personal WBAN as well as an individual sensor and its parent device, (d) maintain the integrity of sensor data from initial acquisition to final storage, and (e) protect access to stored data or data in transit.
On the security front, the options that exist for user authentication. First, fingerprint scanners are now available on PDAs as well as PC cards that can interface with handheld computers. Bar code, RFID tag, magnetic stripe, and smart card technologies offer alternatives.
Wireless links must therefore transfer encrypted data. Security and privacy protection mechanisms use a significant part of the available energy and should therefore be energy efficient and lightweight. Thus security needs create significant challenges. Fortunately, one advantage of WBAN environments is that the very short communication ranges (several meters) aid secure communication
e) Intelligence - The level of local-signal processing capability determines how much power is available, the flexibility needed in the signal processing algorithm, how many nodes are in the network and the bandwidth of the signals of interest. Thanks to continued progress in lowering the power consumption of embedded microprocessors, nodes are becoming more and more intelligent.
f) Usability - In most cases, a WBAN will be set up in a hospital by medical staff, not by ICT engineers. Consequently, the network should be capable of configuring and maintaining itself automatically, i.e. self-organization and self maintenance should be supported. Whenever a node is put on the body and turned on, it should be able to join the network and set up routes without any external intervention. The self-organizing aspect also includes the problem of addressing the nodes. An address can be configured at manufacturing time (e.g. the MAC address) or at setup time by the network itself. Further, the network should be quickly reconfigurable, for adding new services. When a route fails, a backup path should be set up. The devices may be scattered over and in the whole body. The exact location of a device will depend on the application, e.g. a heart sensor obviously must be placed in the neighbourhood of the heart, a temperature sensor can be placed almost anywhere. Researchers seem to disagree on the ideal body location for some sensor nodes, i.e. motion sensors, as the interpretation of the measured data is not always the same. The network should not be regarded as a static one. The body may be in motion (e.g. walking, running, twisting etc) which induces channel fading and shadowing effects. The nodes should have a small form factor consistent with wearable and implanted applications. This will make WBANs invisible and unobtrusive.
g) Data Rates - Due to the strong heterogeneity of the applications, data rates will vary strongly, ranging from simple data at a few kbit/s to video streams of several Mbit/s. Data can also be sent in bursts, which means that it is sent at higher rate during the bursts. The data rates for the different applications calculated by means of the sampling rate, the range and the desired accuracy of the measurements. Overall, it can be seen that the application data rates are not high. However, if one has a WBAN with several of these devices (i.e. a dozen motion sensors, ECG, EMG, glucose monitoring etc.) the aggregated data rate easily reaches a few Mbps. The reliability of the data transmission is provided in terms of the necessary bit error rate (BER) which is used as a measure for the number of lost packets. For a medical device, the reliability depends on the data rate Low data rate devices can cope with a high BER (e.g. 10-4 ), while devices with a higher data rate require a lower BER (e.g. 10-10) The required BER is also dependent on the criticalness of the data.
h) Scalability - For patient monitoring it is often necessary to change the number of WBAN nodes to collect various physiological data from a patient. A scalable WBAN will allow to reconfigure WBAN by either adding or removing nodes in the MAC layer design.